Rashes often seem unfathomable to parents. They are amazingly common, unfortunately more so in some children than others, and only a very tiny few are really serious, demanding immediate medical attention.
To guide you, I am going to suggest evaluating a relatively small number of characteristics:
Does the rash blanch or not?
When you press on the suspicious spots for a few seconds, and then let go, do they get much lighter, almost white (blanching), and then within a few more seconds, return to their original color, typically red? Most rashes blanch. What don’t blanch are bruises (the blood has leaked into the skin, and can’t be pushed around with pressure), and very tiny versions of bruises, called petechiae.
Petechiae, which over a very short period of time can rapidly spread, and enlarge into larger spots, appearing as bruises, are associated with a very serious, and if untreated, often rapidly fatal condition, called Meningococcemia. In my entire 34-year career and 3 years of training, I’ve seen about 6-8 cases, the last many years ago. My point here is not to scare you, but make you realize that under the entirely more likely event that the rash in your child does blanch, you can stop worrying about that. Only if you’re not sure should you immediately call for medical help. And remember, the kids with the bad petechial rash look VERY ill: they often don’t respond well to when you talk to them, they appear out of it, may appear very pale, usually have fever. So if your child has no fever, looks bright and alert, this isn’t even on the radar.
Is the rash smooth or scaly when you gently run your finger over it?
My Dermatology professor, Peter Lynch, used to joke that most doctors thought there were two kinds of rashes: “them’s that responded to steroid cream, and them’s that didn’t.” You can quickly become more scientific than that! Rashes caused by irritation of the skin by plants, or fabrics, or chemicals, or a baby’s or toddler’s drool, appear rough to the touch. That is because the top layer of the skin, the epidermis, has been disrupted.
These scaling epidermal rashes, which would include eczema, respond to steroid creams or ointments. My favorite over-the-counter product is hydrocortisone ointment, not cream. First, it’s more potent than a water-based cream, and second, it only has to be applied twice daily to be effective, instead of 4 times a day creams need to be used to help. What’s more, most inexpensive hydrocortisone creams use propylene glycol, as in alcohol, as the vehicle: unfortunately these products will sting if applied to an open sore, and unlike the ointment, should not be used for vaginal rashes.
Rashes on the face, or in the diaper area, where the skin is relatively thin, will respond well to the hydrocortisone ointment, so it can be tried before seeking medical advice. If scaling rashes on the trunk or extremities don’t respond, you may be on the right track, but simply need a stronger steroid ointment. That would be time to see your medical provider.
One last note on scaling rashes: Please use prescription steroids, which can be very potent, for the rash for which they were prescribed, and for the often limited time (7-14 days or less!) specified on the prescription. I have seen a very nasty rash around the mouth caused by use of a potent steroid, prescribed for a leg rash, which was applied for many weeks before my advice was sought.
Smooth rashes involve the living part of the skin, where all the blood vessels are, the dermis. They should always blanch, as noted above, and most commonly are associated with viral infections. During the summer months, the enteroviruses (hand, foot and mouth disease) very frequently produce a scattered, non-itchy, smooth, blanching rash, which the child is unbothered by, and which often occurs late in the illness course, even week 2. (Hence, my description of them as “Sayonara rashes,” as they often herald, “Goodbye, farewell, I’m leaving in the morrow “)
Rashes that occur while taking medications, such as antibiotics, especially if itchy, raise he possibility of an allergic reaction. Any smooth, blanching, itchy red rash that occurs while your child is taking a medication should result in “stop, drop and call.” Stop giving the medication immediately and call your medical provider for advice.
Does the rash itch?
Both epidermal rashes, like severe eczema, as well as dermal rashes such as an allergic reaction to penicillin can be itchy. The good news is that the rapidly fatal meningococcal rash is NOT associated with itching. The itch associated with scaling rashes will respond to steroid ointments, while that associated with smooth rashes won’t. Either, however, can be treated with inexpensive over the counter Benadryl (diphenhydramine). It comes in 12.5 mg per teaspoon liquid, and in 25 mg capsules (dirt cheap at Costco!). Antihistamines should not be used in children under 2 years of age unless a medical provider gives a parent a specific dose. Finally, if your child is miserable despite the diphenhydramine, it is time for an office visit with your provider, to sort out what else can be done for the rash, and to consider a more potent medication for the itching, such has hydroxyzine (Atarax).
Rashes takes years for most medical providers to become comfortable with, so don’t despair if you are still lost! The key advice to leave you with is this: if it doesn’t blanch, seek immediate medical attention. If it does blanch, your child isn’t taking any prescription medications, especially antibiotics, and doesn’t appear feverish or ill, you have time to try something on your own before seeking your medical provider’s help if it’s not improving in a few days to a week. An ill-appearing child with a fever should always be evaluated promptly.

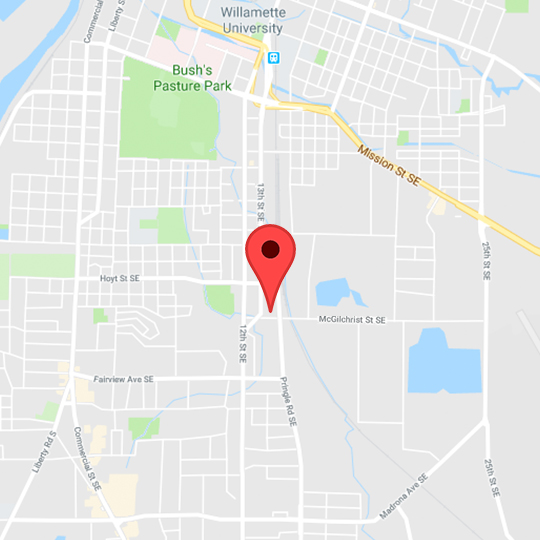
 and then tap "Add to homescreen".
and then tap "Add to homescreen". Salem Pediatric Clinic
Salem Pediatric Clinic